
Applied Science Letters


Background: Breast cancer has become the focus of both healthcare staff and society equally. With the rapid growth of breast cancer incidence around the globe, further considerations including awareness campaigns and annual screening programs were introduced. Surgeons must be aware and knowledgeable when they encounter patients, as early detection is directly related to better outcomes. Objectives: We aimed to review the literature reviewing breast cancer, pathophysiology, risk factors, clinical presentation, diagnosis, management, and prognosis of this disease. Methodology: PubMed database was used for article selection, and the gathered papers had undergone a thorough review. Conclusion: Breast cancer risk profile is crucial for the target population of breast cancer, as it predicts the pattern of developing the disease in the family. Triple assessment, including clinical examination, radiological findings, and histopathological results, is the protocol for making a diagnosis of breast cancer. Treatment of breast cancer depends on the stage and the options include breast-conserving therapy or mastectomy along with radiation, chemotherapy, and hormonal treatment.
An Overview on Diagnosis and Management Approach of Breast Cancer
Emad Ahmad Alnoqaidan1, Renad Mohammed Rubui2, Abdulrhman Salem Alshehri3, Zaid Fayez A Aljarba4, Nader Nasser G Alhelali5, Ahmed Saud Aldablan6, Athari Za’al Albalawi7*, Assaf Hassan A Alamri6, Ammar Salahuddin Shaaban8, Amar Tarik Albaghdadi 9
1 Department of Surgery, King Fahad Specialist Hospital, Qassim, KSA
2Faculty of Medicine, Ibn Sina National College of Medicine, Jeddah, KSA
3Faculty of Medicine, Umm Al Qura University, Makkah, KSA
4Faculty of Medicine, Jordan University of Yarmouk, Irbid, Jordan
5General Practitioner, Alsafiyah Health Center, Medina, KSA
6Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan
7Faculty of Medicine, Tabuk University, Tabuk, KSA
8Faculty of Medicine, southeast university, Nanjing China.
9 Plastic Surgery Department, King Fahad General Hospital, Jeddah, KSA
ABSTRACT
Background: Breast cancer has become the focus of both healthcare staff and society equally. With the rapid growth of breast cancer incidence around the globe, further considerations including awareness campaigns and annual screening programs were introduced. Surgeons must be aware and knowledgeable when they encounter patients, as early detection is directly related to better outcomes. Objectives: We aimed to review the literature reviewing breast cancer, pathophysiology, risk factors, clinical presentation, diagnosis, management, and prognosis of this disease. Methodology: PubMed database was used for article selection, and the gathered papers had undergone a thorough review. Conclusion: Breast cancer risk profile is crucial for the target population of breast cancer, as it predicts the pattern of developing the disease in the family. Triple assessment, including clinical examination, radiological findings, and histopathological results, is the protocol for making a diagnosis of breast cancer. Treatment of breast cancer depends on the stage and the options include breast-conserving therapy or mastectomy along with radiation, chemotherapy, and hormonal treatment.
Keywords: Breast cancer, Management, Mastectomy, Risk factor, Prognosis, Chemotherapy.
INTRODUCTION
Breast cancer is the center of attention when it comes to women’s cancer, as it is the most frequently diagnosed life-threatening cancer in both developed and developing countries [1-4]. Furthermore, it is the leading cause of cancer-related death in women in the latter. [5] A recent paper suggested that the prevalence of breast cancer among Saudi women is high with 21.8%. [6] The anatomy of breast structure is important to differentiate between malignant and benign tumors and even the subtypes of malignancies. The breast consists of fifteen to twenty lobes of glandular tissue that are surrounded by connective and adipose tissue. Each love is divided into tubule-alveolar glands lobules. Lobes have common estuaries named lactiferous ducts that dilate into sinuses and open into nipples. Hence, Breast malignancies can be broadly classified into lobar or ductal. This paper aimed to review breast cancer and its risk factors, diagnosis, and management.
METHODOLOGY
PubMed database was used for the selection process of relevant articles, and the following keys used in the mesh ((“Breast cancer"[Mesh]) AND (“Diagnosis"[Mesh] OR "Management"[Mesh] OR "Risk factors"[Mesh])). For the inclusion criteria, the articles were selected based on including one of the following: Breast cancer or risk factors, evaluation, management, prognosis, and diagnosis. Exclusion criteria were all other articles that did not meet the criteria by not having any of the inclusion criteria results’ in their topic.
Review:
Breast cancer is clinically categorized into stages based on TNM classification which stands for tumor, node, and metastasis. Assessment based on the clinical features and size of the tumor (T), the number of regional lymph nodes involved (N), and whether distant metastases have occurred or not (M). Table 1 shows the exact description of the TNM classification. Accordingly, the surgeon can decide to determine the stage of the current tumor. The stages range from I to IV relative to the corresponding TNM classification. Table 2 shows the possible TNM combination for each stage. [7]
Table 1. Tumor-Node-Metastasis Classification in Breast Cancer
|
Tumor (T) |
|
|
Tx |
Primary tumor cannot be assessed |
|
T0 |
No evidence of primary tumor |
|
Tis |
Carcinoma in situ: ductal, lobar, or Paget disease of nipple with no tumor |
|
T1 |
Tumor ≤2 cm in greatest dimension |
|
T2 |
Tumor >2 cm but ≤5 cm in greatest dimension |
|
T3 |
Tumor >5 cm in greatest dimension |
|
T4 |
Tumor of any size that directly extends into the chest wall (except for pectoralis muscle), skin ulceration or edema, satellite skin lesions, or inflammatory carcinoma. |
|
Lymph Nodes (N) |
|
|
Nx |
Lymph nodes cannot be assessed |
|
N0 |
No histological evidence of regional lymph node metastases |
|
N1 |
Metastases in 1—3 axillary nodes or internal mammary nodes with microscopic disease evident by biopsy |
|
N2 |
Metastases in 4—9 axillary nodes or clinically apparent disease internal mammary nodes |
|
N3 |
Metastasis in ≥10 or more axillary lymph nodes, in infraclavicular or supraclavicular lymph nodes, or clinically apparent ipsilateral internal mammary lymph nodes or in the presence of ≥1 positive axillary lymph node with negative microscopic metastasis in internal mammary lymph nodes. |
|
Metastases (M) |
|
|
Mx |
Distant metastases cannot be assessed |
|
M0 |
No distant metastases |
|
M1 |
Distant metastases |
Table 2. American Joint Committee on Cancer stage groupings
|
Stage |
TNM combination |
|
Stage 0 |
Tis, N0, M0 |
|
Stage I |
T1, N0, M0 |
|
Stage IIA |
T0, N1, M0 T1, N1, M0 T2, N0, M0 |
|
Stage IIB |
T2, N1, M0 T3, N0, M0 |
|
Stage IIIA |
T0, N2, M0 T1, N2, M0 T2, N2, M0 T3, N1, M0 T3, N2, M0 |
|
Stage IIIB |
T4, Any N, M0 Any T, N3, M0 |
|
Stage IV |
Any T, Any N, M1 |
Pathophysiology
Breast cancer, as any others, emerges as a faulty DNA sequencing that is usually prone to estrogen effect; some genes are inheritable like BRCA1 and BRCA2. [8] The histopathological classification sort malignancies according to their invasiveness, invasive or in situ, and their response to hormones, estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). [9, 10] The Cancer Genome Atlas Network (TCGA) set four main subtypes of breast cancer according to the genetic and histopathological qualities: luminal A, luminal B, basal-like, and HER2-positive. [11]
Risk Factors
The possibility of developing breast cancer succumbed to different variables where some are predetermined and non-changeable and some are not. Gender, as a fixed factor, plays a key role in breast cancer, the incidence rate of women breast cancer is around 122 in 100,000 while less than 1 in 100,000 in men. [12] Also, age affects a bimodal distribution with two peaks; one at the age of 50 and the other at the age of 70. [13] As mentioned previously, some DNA abnormalities can be passed through generation, women with a history of one affected first-degree relative have a 1.8-fold increased breast cancer risk. Moreover, women with two or three affected relatives have a 2.9-fold and a 3.9-fold increased risk, respectively. [14] Prior history of breast cancer in the patient is an independent risk factor itself, the chances of contralateral breast cancer in those patients are three to four times compared to the general female population. [15] Prolonged exposure to estrogen, whether endogenous due to nulliparity, early onset of menses, and late age of menopause or exogenous like contraceptive and hormonal replacement therapy HRT, exhibited an increased risk of developing breast cancer. [16, 17] Modifiable risk factors related to both environment and lifestyle. Obesity, smoking, alcohol consumption, and dietary habits all were correlated to malignancies in general and breast’s in particular. [18-21]
Clinical Presentation
A competent surgeon should explore all the aforementioned areas of history, as it will help in developing a good screening method and schedule. History must include detailed obstetric and gynecology history along with previous malignancies in oneself and family members. As the tumor might not be easily detected by the patient, women must be encouraged and educated by their general practitioner about self-examination. An American study suggested that up to 25% of the breast cancer cases were detected about the patient upon self-assessment. [22] The most common symptoms reported by the patients are breast lump (83%), nipple abnormalities (7%), breast pain (6%), and breast skin abnormalities (2%). [23]
Diagnosis
Diagnosis of breast cancer mandate triple assessment; clinical evaluation, imaging, and tissue biopsy. Trained surgeons can detect abnormal signs upon a physical examination which include, but are not limited to an inspection of nipple and skin changes and palpation of breast parenchyma and lymph nodes. Table 3 explains the highlights of breast inspection and palpation. [24]
Imaging techniques used in both screening and diagnosis of breast cancer are mammography, ultrasonography, and magnetic resonance imaging. Albeit mammography is the initial radiological test for screening. It is used to affirm the findings of physical examination and explore the possibility of other non-palpable masses. Furthermore, it helps in examining heavy and large breasts which are difficult to physically examine. Ultrasonography is mainly used to identify the presence of cyst after mass confirmation by mammography, especially in non-palpable and deep-seated masses. Last but not least, MRI's main rule is to shed light on neovascularization areas that surround growing tumors. Likewise, contrast-enhanced MRI sensitivity to small lesions is up to 100%, especially when it comes to distinguishing recurrence from scar tissue. [7]
Two methods are in use for tissue biopsy; fine-needle aspirations and core needle aspiration biopsies. Fine needle aspiration warrants accurate results in diagnosing malignancies if the surgeon is skilled. On the other hand, core biopsy displays information about the nature of the tumor and whether it is invasive or non-invasive. In small lesions, less than 1 cm, the needle can push the tumor aside unless the breast was stabilized and compressed like in X-ray guided procedures. [7]
Table 3. Breast examination remarks
|
Inspection |
Nipple: Asymmetry, obvious masses, and discharge |
|
Skin: Discoloration, dimpling, erythema, peaud' orange, and visible vessel engorgement |
|
|
Palpation |
Lymph nodes: Palpate cervical, supraclavicular and axillary lymph nodes group Document size, number, and mobility |
|
Breast Parenchyma: Palpate four breast quadrant along with subareolar “central quadrant” Document size, shape, location, consistency, and mobility |
Management
The management plan depends on the patient’s current stage, overall physical and mental health. Respecting the autonomy of the patients and explaining the options is the first thing to consider when designing the pathway. Surgery and radiation are the mainstay treatment of breast cancer along with adjuvant hormone or chemotherapy. The decision is made based on the clinical judgment of the surgeon’s side to side with the tumor staging. Surgical options include breast-conserving therapy and mastectomy. Breast-conserving therapy (BCT) is further subclassified into lumpectomy: where a small amount of the surrounding tissue is removed; wide excision: in which a larger amount of the surrounding normal tissue is removed; and quadrantectomy: as the effected one-fourth of the breast is excised. Mastectomy options are total mastectomy (TM) or simple mastectomy: removal of the breast tissue, skin, areola, and the nipple and; skin-sparing (SSM): similar to TM except for leaving as much skin as possible for possible reconstruction; modified radical mastectomy (MRM): similar to TM but confined to the continuity of axillary lymph node dissection. [24, 25]
BCT, unless contraindicated, consider the optimum options for the early stages of breast cancer as it showed similar equivalent survival and recurrence outcomes. Absolute and relative contraindications are enlisted in Box 1. Despite surgical margins of excision not agreed upon among surgeons, BCT was considered successful if histopathological negative surgical margins were obtained as it is associated with low local recurrence. Removing the involved axillary lymph node is part of the surgical excision of breast malignancies. Complete axillary lymph node dissection (ALND), or removal of level I and II axillary nodes used to be the standard procedure with all invasive breast cancers. Nowadays, sentinel lymph node (SLN) biopsy can be attained during the surgery, and dissection of only affected lymph nodes are done, sparring the patient the unpleasant side effects of ALND. Figure 1. Demonstrate levels of axillary lymph nodes. [24, 26]
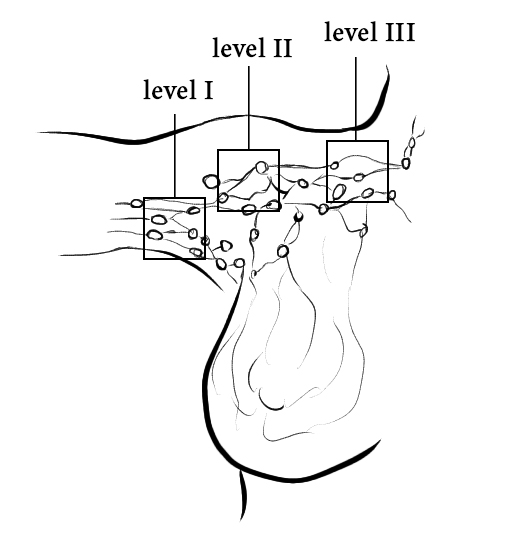
Figure 1. Three levels of axillary lymph nodes. Low axilla (level I), mid axilla (level II), and high axilla (level III).
|
Box 1. Contraindication of breast-conserving therapy Absolute Multicentric disease (involvement of more than one quadrant) Diffuse malignant-appearing calcifications Inflammatory breast cancer Prior radiation to the chest or breast Inability to receive radiation Failure to obtain negative margins after BCT Pregnancy Relative Skin dimpling Nipple and areolar retraction Tumor location |
Radiotherapy is used to target a tumor or post-surgery tumor site. As the radiation works very effectively in extinguishing cancer cells that may linger after surgery when negative margins are obtained. Radiation therapy is an essential part of BCT, while its use is limited in the postmastectomy case to those who suffer from advanced stages to prevent a recurrence. The high dose treatment is given in over five to seven weeks, five days a week, 15 minutes for each session. [25, 26]
Chemotherapy can be used both as a neoadjuvant or adjuvant agent. The specific choice of what pharmacological agent would be based on the patient’s health, medical history, type and stage of the tumor, and obstetric history, etc. Neoadjuvant chemotherapy is used to downstage the tumor in the breast and auxiliary lymph node involved, hence promote the chance of breast conservation and avoiding ALND. Chemotherapy usually is given in cycles, followed by a recovery period. Cycles are given in intervals of two to three weeks in a “dose-dense” manner. Adjuvant therapy includes both chemotherapy and hormonal treatment. The choice of which agent is highly dependent on hormone receptor positivity or negativity and expression of HER-2. The primary goal of adjuvant therapy is the enhance disease-free survival and overall survival rates. [24-26]
Prognosis and life quality
The prognosis of breast cancer patients can be better explained by the multifactorial model. The number of lymph nodes involved, tumor size, TNM staging, and ER, PR, HER-2 responsiveness status can significantly predict the 5 years, 10 years, and 15 years disease-free survival. Smaller tumors, the fewer number of lymph nodes involved, positive hormonal receptors, and early staging were associated with better outcomes. While the opposite, in addition to HER-2 expression, forecast poor prognosis. [27]
CONCLUSION
Breast cancer depends on the triple assessment for making a diagnosis. But taking a detailed history that covers all the possible risk factors can guide the way for the practitioner to either include or exclude the possibility of breast cancer. The presentation of breast cancer varies as apparent palpable tumors may present in very late stages. Consequently, a screening program scheduled for the targeted population according to their past medical and family history is recommended. Treatment of breast cancer relies on TNM classification to determine the stage of the malignancy. Management plans include surgery and radiotherapy mainly along with adjuvant and neoadjuvant chemotherapy and hormonal therapy. The decisions of BCT or TM depend on the stage and another variable, hence, a full picture of the current status shall be obtained by the treating surgeons before proceeding. The prognosis and survival of breast cancer can be assessed through different factors including, stage, age, and others.
REFERENCES
